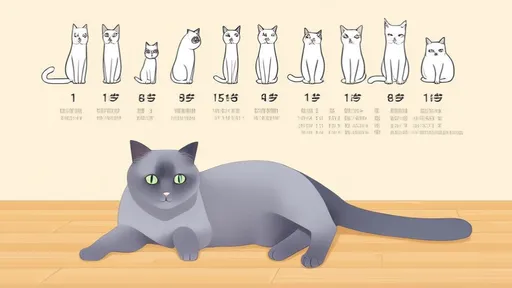
Chronic kidney disease (CKD) is a common yet often overlooked health concern in aging cats. Unlike acute kidney injuries, which manifest suddenly, CKD develops gradually over months or years, making early detection challenging. Many cat owners only recognize the problem when their feline companions show obvious symptoms like weight loss, increased thirst, or lethargy—by which time significant kidney damage may have already occurred. Understanding the subtle early signs, diagnostic approaches, and proactive management strategies can dramatically improve both quality and length of life for affected cats.
The kidneys play a vital role in filtering waste, regulating hydration, and maintaining electrolyte balance. When kidney function declines, toxins accumulate in the bloodstream, leading to a cascade of health issues. What makes CKD particularly insidious is its silent progression; cats are masters at hiding discomfort. Early indicators might include slightly increased water consumption or more frequent urination—changes easily dismissed as benign. Veterinarians emphasize the importance of routine bloodwork and urinalysis for senior cats, as these tests can reveal elevated creatinine or dilute urine long before outward symptoms appear.
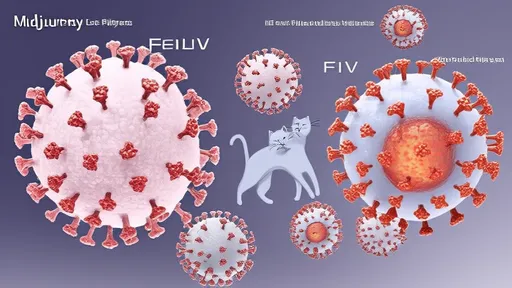
Diagnosing CKD requires a multifaceted approach. Blood tests measuring symmetric dimethylarginine (SDMA) have revolutionized early detection, often identifying kidney dysfunction months earlier than traditional creatinine tests. Urine-specific gravity helps assess the kidneys' concentrating ability, while protein-to-creatinine ratios screen for protein loss. Imaging tools like ultrasound can reveal structural abnormalities such as shrunken or irregularly shaped kidneys. These diagnostic tools, combined with a cat's clinical history, create a comprehensive picture of renal health. The International Renal Interest Society (IRIS) staging system helps classify disease severity, guiding treatment plans tailored to each cat's needs.
Nutrition forms the cornerstone of CKD management. Phosphorus restriction becomes crucial as compromised kidneys struggle to excrete this mineral, leading to secondary hyperparathyroidism. Therapeutic kidney diets are formulated with reduced phosphorus, high-quality protein, and added omega-3 fatty acids to combat inflammation. While some cats resist dietary changes, gradual transitions mixed with appetite stimulants or feeding tubes in severe cases can ensure proper nutrition. Hydration support through subcutaneous fluids given at home often dramatically improves energy levels and appetite. Many veterinarians recommend water fountains or adding broth to food to encourage voluntary fluid intake.
Beyond diet, medication management addresses CKD's systemic effects. Potassium supplements may be necessary for cats with low blood potassium levels, while binders like aluminum hydroxide control phosphorus absorption from food. Anti-nausea medications and acid reducers alleviate common gastrointestinal symptoms. Erythropoietin injections combat anemia resulting from diminished kidney hormone production. Regular blood pressure monitoring is essential, as hypertension can accelerate kidney damage—medications like amlodipine help protect remaining kidney function. These interventions, combined with stress reduction at home, create a supportive environment for cats with CKD.
The emotional toll on pet owners managing a cat's CKD shouldn't be underestimated. The financial commitment of ongoing treatments and the emotional labor of daily caregiving can feel overwhelming. However, many cats stabilize remarkably well with proper management, enjoying good quality of life for years after diagnosis. Support groups and veterinary nutritionists provide invaluable guidance for navigating treatment options. As research advances, emerging therapies like stem cell treatment offer hope for further prolonging kidney function. Ultimately, early detection paired with a comprehensive care plan allows many CKD cats to thrive far beyond initial expectations.

By /Jun 28, 2025

By /Jun 28, 2025

By /Jun 28, 2025

By /Jun 28, 2025

By /Jun 12, 2025

By /Jun 12, 2025
By /Jun 12, 2025

By /Jun 12, 2025
By /Jun 12, 2025

By /Jun 12, 2025

By /Jun 12, 2025
By /Jun 12, 2025

By /Jun 12, 2025

By /Jun 12, 2025

By /Jun 12, 2025

By /Jun 12, 2025

By /Jun 12, 2025